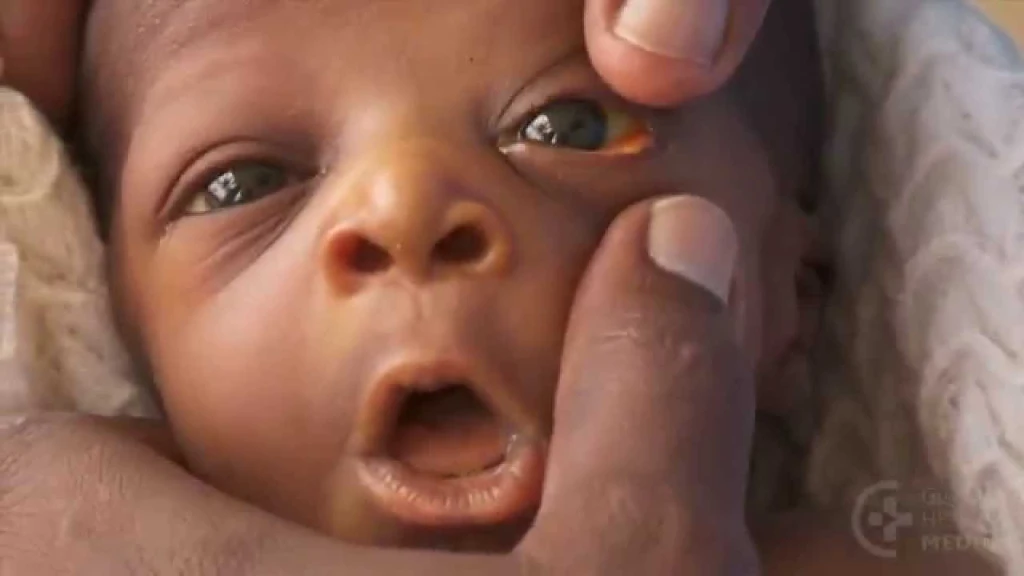
Neonatal jaundice, the yellowish discoloration of the skin and eyes caused by high levels of bilirubin in the blood, has long been recognized as a common condition among newborns.
However, recent clinical observations and reports suggest that the condition appears to be more pronounced and alarming in babies born through caesarean sections compared to those delivered vaginally.
This growing concern demands attention because of the potential health risks jaundice poses if not detected and managed early.
In a close up with 𝐫𝐞𝐧𝐨𝐰𝐧𝐞𝐝 𝐨𝐛𝐬𝐭𝐞𝐭𝐫𝐢𝐜𝐢𝐚𝐧 𝐚𝐧𝐝 𝐠𝐲𝐧𝐚𝐞𝐜𝐨𝐥𝐨𝐠𝐢𝐬𝐭 𝐃𝐫. 𝐉𝐁 𝐅𝐨𝐫𝐝𝐣𝐨𝐮𝐫 𝐢𝐧 𝐒𝐮𝐧𝐲𝐚𝐧𝐢, he explained several factors behind this increased risk. One factor is the administration of anti-malarial drugs, specifically 𝐬𝐮𝐥𝐟𝐚𝐝𝐨𝐱𝐢𝐧𝐞-𝐩𝐲𝐫𝐢𝐦𝐞𝐭𝐡𝐚𝐦𝐢𝐧𝐞 (𝐒𝐏), to mothers during antenatal care. In some cases, mothers with a 𝐆𝟔𝐏𝐃 deficiency—a genetic condition affecting red blood cells—may be mistakenly given these medications, worsening the baby's bilirubin levels.
Another cause relates to the birthing procedure itself, during caesarean section deliveries, cutting the umbilical cord can sometimes push excessive blood into the baby, increasing the breakdown of red blood cells and leading to higher bilirubin production.
Prenatal infections, including sexually transmitted diseases left untreated could also contribute to the risk of jaundice in newborns. Dr. Fordjour emphasized that if high bilirubin levels are not treated promptly, it can result in a serious condition called 𝐤𝐞𝐫𝐧𝐢𝐜𝐭𝐞𝐫𝐮𝐬, which can cause brain damage in babies.
He mentioned, to manage neonatal jaundice, affected infants are typically placed under specialized "social lights" (phototherapy) that help detoxify the bilirubin in their bodies whereas mild cases could be corrected by regularized breastfeeding.
He explained that in the past, more invasive treatments such as exchanged blood transfusions—where the baby's blood is replaced with the mother’s were used to correct severe cases.
This insight highlights the importance of careful prenatal care and monitoring of newborns delivered through the caesarean section to prevent and treat neonatal jaundice effectively.
One major factor lies in delayed initiation of breastfeeding among babies delivered through the caesarean section. Unlike vaginal deliveries where the newborn is often placed on the mother’s breast within the first hour, caesarean births sometimes lead to prolonged separation of mother and child due to post-surgical recovery and maternal discomfort.
Early and frequent breastfeeding plays a critical role in flushing out bilirubin through stool and urine. When feeding is delayed or inadequate, bilirubin builds up in the baby’s system, increasing the likelihood of jaundice.
Although these factors may not be the definitive causes, he explained that medical practitioners are still conducting research to find the exact cause, as neonatal jaundice similarly occurs in some cases of spontaneous vaginal delivery (SVD).
A visit to the Mother and Baby Care Unit (MBU) at Sunyani Teaching Hospital reveals the emotional weight carried by mothers who have undergone caesarean sections and whose babies are suffering from jaundice. The confusion and concern are evident on their faces as they navigate this challenging time. Often, these mothers face longer hospital stays, with their newborns spending extended periods in the Neonatal Intensive Care Unit (NICU) to receive the specialized treatment needed to manage the condition.
The alarming rise of neonatal jaundice in caesarean-born babies is therefore not just a medical issue but also a maternal and neonatal care challenge.
In conclusion, while caesarean sections are often life-saving, the heightened risk of neonatal jaundice among these babies cannot be ignored.
Sompaonline/𝐋𝐚𝐰𝐫𝐞𝐧𝐜𝐞 𝐘𝐞𝐛𝐨𝐚𝐡 𝐆𝐲𝐚𝐧
𝐍𝐞𝐨𝐧𝐚𝐭𝐚𝐥 𝐉𝐚𝐮𝐧𝐝𝐢𝐜𝐞: 𝐀 𝐆𝐫𝐨𝐰𝐢𝐧𝐠 𝐂𝐡𝐚𝐥𝐥𝐞𝐧𝐠𝐞 𝐟𝐨𝐫 𝐂𝐚𝐞𝐬𝐚𝐫𝐞𝐚𝐧 𝐒𝐞𝐜𝐭𝐢𝐨𝐧 𝐁𝐚𝐛𝐢𝐞𝐬